The most common causes and strategies for preventing shoulder pain
Shoulder pain is very common as we lead a combination of sedentary, desk based lives with the occasional hour or two of vigorous exercise thrown into the mix every week. To follow is a focus on the most common cause and strategies for preventing shoulder pain.
The three most common causes are ;
- Injury through a specific incident – either a fall, sport related or not,
- Overuse either with gradual onset due repetition of a specific movement either with sport or life in general
- And also pain due to Osteoarthritis within the shoulder joints.
The second category is the one most often seen in practice and so it will be the main focus
Symptoms, Cause, Treatment and Preventing shoulder pain
Symptoms
A ‘catching’ pain as the arm is raised either out in front of you or to the side. As the painful point is reached there can be a sense of weakness. As you move past the catching point the pain reduces.
Pain at night and stiffness in the morning on the painful shoulder
A sense of weakness in the gym and a loss of power.
An aching pain into the deltoid at the front or side when the arm is held in a certain position.
If these symptoms sound familiar to you then the following advice and exercises can help. It is often due to inflammation or tear of the one of the tendons in the Rotator cuff muscles. The rotator cuff is a number of muscles that converge around the head of the shoulder joint to give it mobility and stability.

Note: If you have pain at night and reduced movement in all planes of motion then you could have Adhesive Capsulitis or Frozen Shoulder. Please follow this link to read more about how best to treat this condition.
Causes
In our daily lives we spend most of our time with our arms forwards. Either at a desk in front of computers, driving or working with our hands. This brings our shoulders forward and over time muscles at the front such as our pectoral muscles become shorter and muscles at the back of shoulders become stretched.
The stretched muscles highlighted in orange on the image above can become fatigued and the loose their flexibility.
It then only takes something relatively innocuous like a bad night’s sleep on that shoulder, a harder session in the gym, a fall or carrying a heavy bag for a long time for the muscle to tear or a tendon (where the muscle attaches to the bone) to become inflammed.
As these muscles are in constant use, and they are on a stretch as well and blood flow in that area is not great the healing process can take a long time. More often than not the small tear becomes a little bigger and the inflammation becomes greater. And what was a mild discomfort becomes something quite painful.
It’s at this point that many of us go to our GP and get some anti-inflammatories. It helps a bit. We rest it and the pain reduces. We then start using the shoulder more, perhaps return to the gym and the pain returns.
If at this stage the muscle tear is relatively small <5mm then this can heal and physical therapy is best placed to help this. As it is impossible to tell without an MRI GPS recommend rest, anti inflammatories and physio therapy in the first instance. If after this symptoms persist then more often than not an MRI is requested. Based on the findings a specialist can recommend whether surgery is the best option or further physical therapy.
Prevention – Physical therapy & Exercises
In order to prevent shoulder pain we need to address the cause. By reducing the ‘stretch’ by loosening off the muscles that are pulling our shoulders forward.
At the same time you need to reduce the inflammation.
A combination of rest, strong anti-inflammatories and ice will help. Sometimes a steroidal anti inflammatory injection can be very effective.
However you still need to address the cause of the injury.
Addressing the cause of the injury
Reduce the tension and tightness of the internal rotators of the shoulder. The Pectorals, Biceps short head , Teres Major and Subscapularis. This can be done through a combination of soft tissue release massage and exercises designed to return these tight muscles to their longer resting length
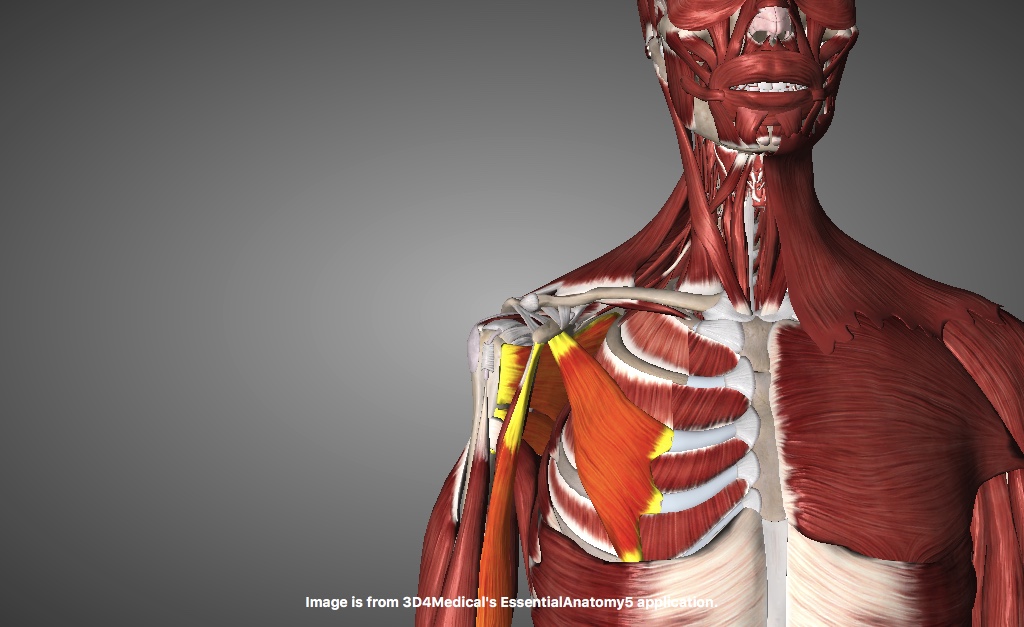
And then combine this with strengthening the external rotators: Teres Minor and Infraspinatus.

The exercises need to be done regularly at least twice per day to offset the inputs we give it for hours at a time at our desks.





 k of the leg can increase from occasionally uncomfortable to very painful.
k of the leg can increase from occasionally uncomfortable to very painful.