Essential Advice for Preventing Neck Pain
If you’ve experienced neck pain, this guide is tailored for you. Discover actionable, expert-backed advice for preventing neck pain, drawing on over a decade of clinical experience from Hugo Firth, a seasoned Osteopath in the Kingston and Surbiton area. With thousands of patients treated, Hugo shares his top five strategies to help you avoid neck pain, blending ergonomic adjustments with targeted therapeutic exercises.
What This Guide Covers:
- Top Causes of Neck Pain: Understanding why neck pain occurs and common contributing factors.
- Lifestyle and Ergonomic Adjustments: Tips to modify daily habits and workstation setup to ease neck strain.
- Effective Exercises for Flexibility: Practical exercises to boost flexibility and minimise future neck pain risk.
Causes of Neck pain
Whilst we hear of disc injuries and arthritis the main cause of neck pain is overworked or fatigued muscles.
What Are Fatigued Muscles?
Fatigued muscles are muscles that have been overworked and have become strained, resulting in reduced functionality and discomfort. Often a patient may say, “All I did was turn my head, and now I can’t move my neck!” This scenario highlights how even a minor movement can become overwhelming for fatigued muscles, leading them to strain and spasm.
Why Do Muscles Fatigue?
The underlying issue often lies in our modern, sedentary lifestyles. Unlike previous generations, most of us spend prolonged hours sitting, both at work and during our commute, followed by more seated time at home watching TV or using digital devices. With these habits, we may sit for over 12 hours a day!
Impact of Modern Activities on Muscle Health
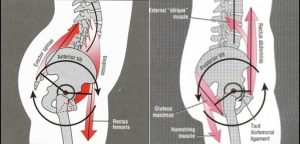
Even popular forms of exercise like cycling or gym workouts can contribute to muscle fatigue if they reinforce postural habits that keep the body in a flexed position (bent at the hips), shoulders and arms forward.
Over time, our bodies may adapt to this position, interpreting it as “normal.” This adaptation leads to weakened neck and shoulder muscles, making them less resilient and more prone to strain when asked to perform basic tasks like turning the head.
So our bodies could be forgiven for thinking that this is our desired position.
Hips flexed, upper back arched, arms forward, head up!
Adaptability of Our Bodies
Our bodies are incredibly adaptable, adjusting to the activities and postures we regularly assume. When we sit for extended periods with arms forward and head up, our bodies adapt to make this position feel normal and sustainable.
How Our Bodies Adjust to Prolonged Sitting:
- Neck Muscles: Constantly contracting to keep our eyes level with a screen, which can lead to chronic tension.
- Upper Back Muscles: These stretch out as we lean forward, potentially weakening over time.
- Pectoral Muscles: Shorten due to the arms being held forward, reinforcing a slouched posture.
While these adaptations allow us to remain in this position comfortably for longer periods, there is a hidden cost.
The Price We Pay for Modern Postures
Our shoulder, upper back, and neck muscles often work in overdrive—sometimes exceeding 12 hours a day in a slightly stretched or contracted state due to prolonged sitting and screen time. This persistent posture strains several key muscle groups that can contribute directly to neck pain and stiffness.
Key Muscles Contributing to Neck Pain
- Sub-Occipital Muscles: These small muscles at the base of the skull stay contracted to keep our eyes level with screens, leading to stiffness, tension, and even headaches.
- Upper Back and Shoulder Muscles: These muscles often remain in fixed positions, experiencing stiffness and tightness due to lack of movement throughout the day. The prolonged strain can weaken these muscles, making them more susceptible to discomfort and pain.
Over time, the continuous strain on these muscles from poor posture and limited movement can lead to chronic pain and reduced mobility, highlighting the physical cost of our modern, sedentary lifestyle.
Preventing Neck Pain Advice #1
Being static involves a lot of work for our neck muscles.
We can change the inputs our bodies receive.
From a ‘be static for 12hrs’ to ‘static for 58 mins then move for 2 mins, repeat x 12!’
If you change the messages that the muscles receive regularly enough during the day the body will adapt.
It will increase blood supply to nerves and muscles and joints. More oxygen and nutrients to muscles means less lactic acid build up and less fatigue.
Neck pain Advice tip # 2
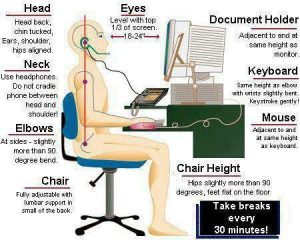
Repetitive turning, looking up or down will increase fatigue in neck muscles
Office
Check your monitor height
If you have more than one screen align the one you use most to be the one in front of you
Turn and face colleagues directly rather than turning your neck
Home
Make sure TV is directly in front of you- not too high or to the side
Neck Pain Advice tip # 3
Sleep is the great muscle recharger. So it’s important for neck muscles to get a good rest
ADVICE TIP NO 3
Get a supportive pillow
You need to have a NEUTRAL spine
Pillow needs to be firm enough and the right height to achieve this
To thin and neck muscles will be contracted one side and stretches on the other
Stop sleeping on your front
Have enough sleep 7-8hrs is ideal. This will give your muscles enough time to recharge for the day ahead.
Advice Tip # 4
Upper Back Exercises that can change your life
(1)Ensure that your upper back maintains its flexibility
As with all exercises watching them is the easy bit. Incorporating them into your daily life takes effort.
(2) Maintain neck rotation mobility and prevent neck pain
This is a great way of maintaining and preventing a tight neck
But if your neck goes into spasm then this will be too painful
Seek the advice of your physical therapist
Advice tip #5
Managing your stress levels
Everyone deals with stress in different ways
It can manifest itself as tension into neck and shoulder muscles
One way to manage it is through exercise or any activity that can stop you thinking about the stress causing issue for 30 mins or longer
Here are some ideas
Go for a walk, paint/sketch, do a jigsaw, build lego, knit, go for a run, read a book, meditate








 24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.
24 interlinking segments that act liked a coiled spring. If a section of the coil stops moving then the sections above and below move more to ensure our bodies can achieve the movement we require. It’s this extra movement of muscles and joints that over time can lead to muscle fatigue and joint inflammation. These are two main symptoms of lower mechanical back pain.
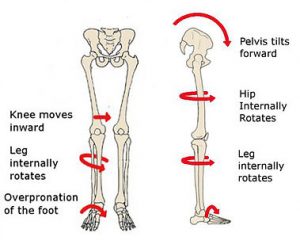 The diagnosis was patella femoral syndrome.
The diagnosis was patella femoral syndrome. Arthritis
Arthritis